The Journal of General Internal Medicine published a study last month that looked at primary care medical practices in Massachusetts to see how well they were able to provide the quality improving capabilities of Patient-Centered Medical Homes. These structural capabilities represent process measures that assess the quality of care in medical practices. However, these same measures could also help patients select their own primary care physicians.
Study Finds Larger Practices Have More Quality Related Capabilities
Not surprisingly the study found that larger practices, (and to a lesser extent those affiliated with larger networks of practices), provided more capabilities to improve the quality of patient care. The most significant difference in capabilities was seen in practices with 5 or more physicians, and these included:
- Practice meets to discuss quality more frequently than every quarter
- Practice regularly open to provide care on weekends
- Use of Electronic health records that provide medication list, problem list, and electronic reminders
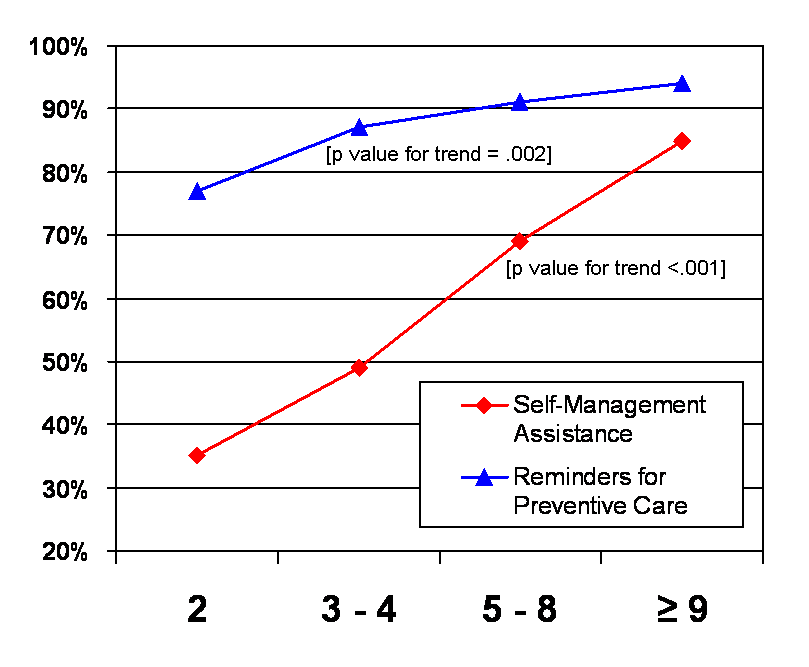
In addition, practices with 9 or more physicians were more likely to have specialty trained staff to assist with patient self-management, and there was an overall trend for larger practices to have reminder systems for preventive care:
 Asking Questions to Improve Quality
Asking Questions to Improve Quality
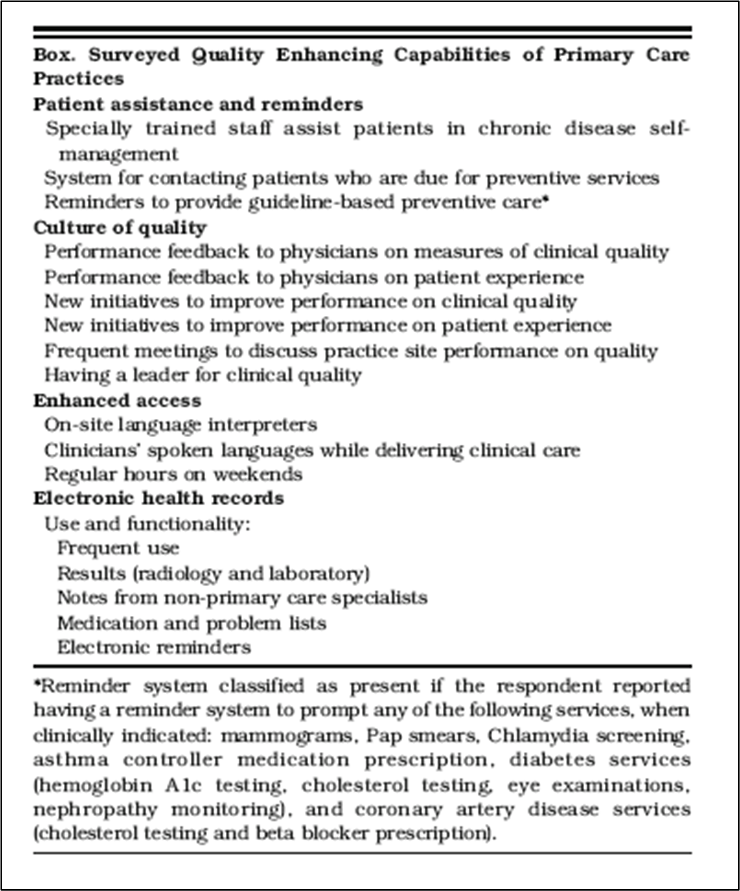
The questions used by the researchers in this study are clearly useful for assessing the quality relate capabilities of primary care practices, but additional research certainly it warranted to determine how well these process measures translate into actual improvements in clinical and economic outcomes. In addition, as such lists are developed and validated further, they could also be used by individuals looking for their own primary care physicians, and by patient advocacy organizations seeking to both promote quality improvement and to “grade” primary care providers.
The specific questions used in the study’s survey was:
One of the challenges for individuals or groups to effectively use any list of this type is that it needs to be customized because they will have different priorities and concerns. For example, the availability of translation services might be important for one family or advocacy organization, but less so for others.
Conclusion
Much has been written about using checklists to improve quality and reduce errors in hospitals – and particularly in the operating room. But perhaps checklists could be derived from this type of Medical Home capabilities survey for use by individual patients and their advocates to assess outpatient clinical sites. While the operating room checklist concept was based upon the airplane pre-flight checklist, maybe the checklist for assessing primary care practices could be likened to the checklist that home inspectors use to help home buyers understand the strengths and problems of a house. If individual patients and their collective advocacy groups regularly used checklists of this type, it could create a significant patient driven force for transforming the structure and operations of outpatient medical care in the United States to improve quality and control costs.

Thanks for your good post.
[…] the integration and consolidation of physicians into larger groups, since it has been shown that larger groups are more likely to be able to provide care coordination and management services to their […]
Good blogs And more informative for Quality of Care in Medical Practices .The Journal of General Internal Medicine information in this article is more informative and very useful……
[…] care (and not just medical services) to patients. These are the types of issues that the “medical home” model tries to encompass by expanding the physician’s responsibility for their individual […]
Thanks Evan – Funding to increase medical home capabilities within (and possibly among) primary care practices/clinics is obviously a very important issue. And one that is complicated by the state of the economy and the other pressing objectives within health reform. But as I think you know, improving the health delivery system at the level of the primary care provider will be a fundamental requirement for actually achieving many of the goals of health reform, e.g., controlling growth in costs and improving quality. In addition, making primary care clinicians more efficient in how they provide care will also help alleviate the shortage of PCPs – something that you know is a big problem here in MA.
Specific funding for medical homes may come from Medicare, (probably via demonstration projects as proposed by MedPAC in their June 2008 report – see Ch 2, and their September Testimony – see http://www.MedPAC.gov). Other sources of funding could come from regional health insurers and hospitals – which in the current economic environment might be the only organizations with the liquidity and interest to fund this type of activity: States, Foundations and employers, are all facing serious fiscal constraints, so are unlikely to come up with financial support in the next year or so.
The other “source” of funding people might point to could be Federal funds to support health IT, including electronic medical records. While EMRs, (or EHRs to some), are one important component of medical home capabilities, making EMRs work to benefit the primary care practice, patients and the overall community is a very difficult task. As many small and medium sized medical practices have found, the time spent learning how to use EMR systems can be quite extensive, and it can take many, many months before the EMR actually increases the office’s operating efficiency – and before then, their efficiency is decreased. Hopefully, the EMR’s value to patients in terms of easier and more accurate retrieval of records, organization of problem lists, medications and allergies, and reminders for preventive care and disease management occurs much quicker – although this is also an open question and likely varies widely from practice to practice and may also depend upon the specific EMR system used.
I realize that this paints a picture which is somewhat of a paradox in that there might not be money to expand primary care capabilities along the lines of medical homes, but that doing so should be a fundamental step to ensure the success of any other broader health reform initiatives. How this is resolved will be important to the long-term success of whatever “health reform” takes in 2009-10, and how smooth or bumpy the implementation of any Federal and State health reforms are in 2010 and beyond.
[For full disclosure, I want to let people know that Evan and I went to school together…. but I didn’t ask him to post the comment – that’s all on him.]
Mike:
Nice blog. this article was informative and raises the questions about the need for appropriate infrastructure and leadership to improve quality. Investment in HIT is having a profound impact on quality yet to capture the benefit, larger practice may be the only ones capable of affording the kind of decision support that is truly helpful.
What do we think is the direction of payment policy will be for these “medical homes”?