Information technology tools has been touted for years as a cornerstone for improving the quality of healthcare and reduce spending. While, clearly this has not been achieved, many e-health initiatives are being launched, and it is unclear how successful or efficient these will be. I am often concerned about the effect e-health systems have on the health care quality when my own physician spends so much time looking into and typing on his laptop. But to avoid discussing the challenges of e-health based upon my n of 1, below are 4 perspectives that are more expansive and analytical:
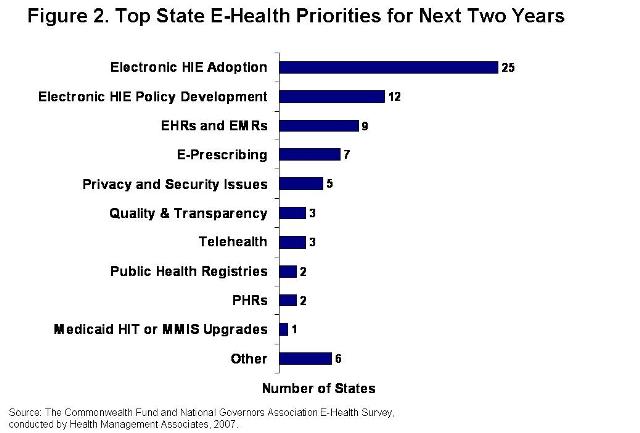
The Commonwealth Fund recently released a report about 27 state governments’ e-health activities in 2007. One remarkable thing about this report is that while there was consensus “that health information technology (HIT) can significantly improve health care delivery and quality and reduce its costs,” states are pursuing a broad range of HIT initiatives:
While Health Information Exchanges (HIEs – which enable the sharing of medical information among clinicians in an area/region), are the highest priority for most states, after that, the consensus starts to break down.
What worries me, is not the lack of activity, but the lack of consistency in implementing any of these systems. I don’t think it would be wise for everyplace to use the same medical records system, etc., but too often the “lets put in an e-health system” decision is supported with a lot of money but without enough up-front time and planning to make the new system actually provide value to patients, clinicians or the overall health system.
The Commonwealth report also has information about the barriers to accomplishing e-health priorities:
- Funding (26 states)
- Stakeholder Impacts, Buy-in (20)
- Establishing Business Case, Sustainability(13)
- Lack of Standards (12)
- Privacy/Security Concerns (11)
- Legal Issues, Technical Resources & Governance Issues (4 each)
The lessons learned by the states were equally diverse:
- Collaboration & Engagement (24 states)
- Time Required (10)
- Communication & Education (8)
- Unknown/Too Early & Funding (7 each)
- Governance, Leadership & Consumer Focus/Involvement (5 each)
Clearly Funding and Collaboration are important. (These are two aspects of health system reform that I am working on in my book project from the perspective of how social and economic forces drive the structure and operations of the US healthcare system.) The importance of the other factors in the Commonwealth report likely depend upon the culture and capabilities of the local health system and healthcare professionals.
The UK National Health Services’ “Choose and Book” system was discussed in the special e-government section in the February 16th issue of The Economist. This system is intended to enable patients and physicians to choose and make appointments for specific services. A couple of bits from this story capture its problems:
- >50% of physicians surveyed by the British Medical Association said that their experience with “Choose and Book” was negative or very negative.
- The doctor interviewed for the piece said that only about one in ten of the appointments she makes with the system turns out fine. And it is slow – consuming up to 2 minutes of a 10 minute appointment – making her a “highly paid and expensively trained doctor who is acting, in effect, as a secretary.”
The City of New York’s is launching a new initiative with $60 million to “equip doctors with computer software that can track patients’ medical records in order to provide better preventive care.” This initiative combines electronic medical records and a local health information exchange. Hopefully, the 2-year prep-time they have spent will enable this initiative to be launched smoothly. And it appears that the NYC health commissioner is setting realistic expectations, since his perspective according to the New York Times is that “medical practices will most likely see a decrease in productivity for about six months as doctors’ offices become familiar with the technology and transfer data from paper records or other systems.”
The Department of Veterans’ Affairs in September 2004 scrapped a multi-million dollar computer system when its installation at the VA hospital in Bay Pines, FL – one of the busiest in the VA system – was deemed a failure. This Core Financial and Logistics System was intended to integrate hospital’s clinical operations with its inventory, budgeting and planning programs. However, it either didn’t work as designed or the VA employees couldn’t understand how to use it – as some of the system’s proponents claimed. In either case the result was the same: Productivity dropped as the number of surgeries that could be scheduled declined, and supplies could not be found. This led to Congressional hearings and Federal criminal investigations about how the tens of millions of dollars spent on this system had been used.
The Bottom Line is that while you can spend a lot of money putting in electronic health systems, getting value from them in terms of more efficient care delivery, better prevention or more efficient financial operations depends a LOT on how the systems are designed and how user friendly they are for both patients and healthcare professionals.
Does anyone else out there have interesting experiences or perspectives on electronic health systems?


[…] Michael D. Miller, MD has something worth reading today (E-Health – A Medical Information Miracle or Mess?)Here’s a brief bit, but follow the link for the rest.In either case the result was the same: Productivity dropped as the number of surgeries that could be scheduled declined, and supplies could not be found. This led to Congressional hearings and Federal criminal investigations about how … […]
[…] Read the rest of this great post here […]
[…] E-Health – A Medical Information Miracle or Mess? The importance of the other factors in the Commonwealth report likely depend upon the culture and capabilities of the local health system and healthcare professionals. The UK National Health Services’ “Choose and Book” system was … […]