“Health insurance reform” has become the latest label for national health reform legislation, but this renaming has pushed discussion about how to transform healthcare delivery farther back into a poorly lit corner of the debate.
Transforming the delivery of healthcare can improve quality and efficiency because the current system has two fundamental impairments: 1) lack of integration and coordination among clinicians and organizations like hospitals, and 2) a shortage of primary care clinicians. There have been many proposals for how to address these structural problems, but they have tended to not be bold enough, i.e., they would take many years – and in some cases decades – to produce significant results.
Listed below are some proposals to address these problems. While all of these are reasonable as individual initiatives, because of the connection between economic incentives and other change drivers in healthcare, integrated approaches that combine multiple changes will work best.
Massachusetts Proposing to Move to ACOs
Massachusetts is considering transforming the state’s entire healthcare delivery system into Accountable Care Organizations (ACOs). These organizations would be structured to better integrate care delivery because all the clinicians and other providers would be within ACOs, (or have contractual relationships with ACOs), and ACOs would also have financial incentives to provide quality and efficiently coordinated care because they would receive risk adjusted global payments for each individual who selected the ACO. It is envisioned that shifting all reimbursement in the state to such global payments would also create incentives for the development of ACOs. The time-frame outlined for creating this ACO-global payment system is 5 years – which seems reasonable.
Medical Homes for Care Coordination
Patient Centered Medical Homes (PCMH) is a model of care delivery where each patient would have a primary care “medical home” practice that would be responsible for providing all their primary care, coordinating their non-primary care and testing, etc., and providing wellness education and self-care management. The concept for the PCMH was originally developed by 4 medical societies, (AAFP, AAP, ACOG, and ACP), and has since been endorsed by many others. The potential of receiving additional payments for providing the care coordination function inherent to a PCMH has attracted great interest from a wide variety of organizations and groups. However, without a generally agreed upon definition for a PCMH, many diluted and divergent definitions have sprung up – presumably to enable whoever developed them to qualify for more money. (I even heard 3rd hand that some pathologists were looking into how to become a medical home. I don’t know if it’s true – maybe they were just looking to understand how they could work with medical homes?)
Several states have begun demonstrations to promote medical homes, and Medicare is scheduled to start a demonstration program next January, but the regulations for implementing this program are about 8 months overdue – perhaps because they didn’t want to start something that would be dramatically altered by health reform legislation.
Medical homes would also certainly be compatible with ACOs, since ACOs would be much more expansive and larger organizations that could include multiple medical homes.
Care Coordination Demonstration Projects and Initiatives
There are many programs for increasing care coordination, from electronic medical records and HIT to facilitate the sharing of medical information, to Medicare pilots to see how case managers could help control spending in traditional (i.e. fee-for-service) Medicare. These initiatives would all be slowly or minimally effective because they are being implemented on top of the existing fee-for-service structure and non-integrated delivery systems. For example, the results of a large Medicare demonstration project showed almost no benefit from 15 different care coordination pilot sites – primarily because the nurse case managers were separate from, (i.e. not integrated into), the physician’s offices.
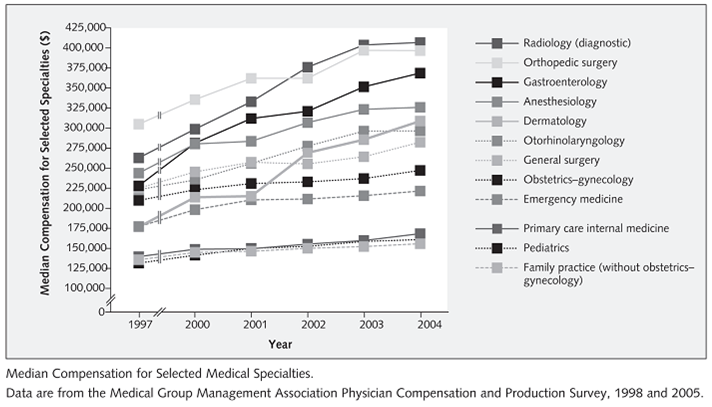
Similarly, the Federal stimulus bill earlier this year included significant funding for implementing electronic medical records in physicians offices. This seems like a good idea since estimates are that less than 10% of physicians offices have such systems. However, the provision was written as a percentage add-on payment to the physician’s Medicare and Medicaid reimbursements. The problem with this structure is that buying EMR systems requires a significant up front outlay of tens of thousands of dollars, and the types of physicians who have typically been paid the least, (i.e. primary care physicians), will therefore be the least able to afford these up front costs. And because they are paid the least, they will also benefit the least from the percentage add-on to their Medicare and Medicaid reimbursements. Conversely, specialists physicians – who have been paid more – will be better able to afford the up front costs of the EMR systems, and will also get the most benefit from the Medicare/Medicaid add-on. (See graph below of average physician compensation by specialty.)
I suspect the provision was structured this way because it was easy, (i.e. it wouldn’t require any additional payment structure – it would just increase the size of payments to physicians through Medicare and Medicaid), the money wouldn’t begin flowing from the Treasury until 2011, and the provision phases out the “carrot” to become a “stick,” i.e. it provides add-on payments in years 2011-14 , but these decrease each year and are replaced by payment reductions for physicians who don’t have EMR systems after 2014. (Note – only EMR systems that meet a “meaningful use” standard will qualify for the additional payments.)
Increasing the Number of Primary Care Clinicians
The American College of Physicians released a white paper in April, and Chapter 1 in the Medicare Payment Advisory Commission’s (MedPAC) June annual report to Congress both address the shortage of primary care physicians. Each of these include proposals focused primarily on using economic incentives to encourage more medical students and residents to choose to go into primary care, to require hospitals to increase the number of primary care residency slots, and to increase residents’ exposure to community based primary care settings. (An additional resource, is a new Kaiser Family Foundation web-based Issue Brief on “Primary Care Shortage”)
Some of the specific proposals from the ACP and MedPAC are:
- Establish a National Health Care Workforce Policy and Commission
- Increase funding for scholarships and loan repayment programs for primary care physicians
- Increase residents’ formal instruction and experience in multidisciplinary teamwork, cost awareness in clinical decision making, comprehensive health information technology, and patient care in ambulatory settings to better align their training objectives and content with delivery system reform
- Realign hospitals financial incentives, (both for Medicare’s educational support and for workforce supply), to increase residents’ non-hospital based experiences
- Improve the quality of practice life for physicians by reducing administrative and paperwork burdens
- Increase reimbursement for primary care physicians so that they are competitive with other types of medical practices. (See below for graph and additional commentary.)
(From: ACP White Paper, “Solutions to the Challenges Facing Primary Care Medicine”)
While all of these make sense, they would take many years, and even decades, to significantly shift the healthcare delivery system’s dynamics toward primary care. Therefore, below are some other ideas for increasing the supply of primary care physicians sooner:
Additional Ways to Increase Primary Care Physician Services:
- Retraining Physicians. Create retraining programs for physicians who haven’t been engaged in clinical work for a while, (e.g. research or administration), or who have been doing mostly specialty care and now want to go into primary care. Some will ask why these physician would want to do this given the current compensation differences between primary care physicians and specialists? – This is why other provisions that create incentives and decrease that gap would be important. (There’s also the issue of board certification for these newly entering PCPs, but that’s a bigger discussion about the role of specialty boards, etc.)
- Direct Support for EMRs. As noted above, the Federal stimulus bill provides financial incentives, (and later financial penalties), for physicians to use EMRs. A better – although more complicated approach – would be to provide grants or zero interest loans to primary care physicians. These would provide financial incentives and support to physicians who needed it the most, and provide additional support to pediatricians who generally don’t bill Medicare very much. In addition, getting more primary care clinicians equipped with EMRs would promote more integration, coordination of care, and efficiency of care delivery across the entire healthcare system, as well as highlighting the importance and prestige of primary care physicians – something that will be important for increasing their numbers in the future. (See below.)
- Increasing Prestige of Primary Care. Increasing the visible prestige of primary care clinicians in the medical and general community could help encourage medical students and resident to become primary care physicians, as well providing indirect support for existing PCPs. For example, hospitals could give them preferred or valet parking, cities could give them placards for free parking at meters and city owned lots, and states could give the children of primary care clinicians free tuition at state universities. Many programs have been developed to recognize the public contribution of groups such as veterans, firemen and policemen, so perhaps some of those could be adapted to publicly recognize primary care clinicians.
- Increasing Supply and Use of Hospitalists. While many specialists wouldn’t want to become primary care clinicians, there is also a need for more physicians to focus on the complex care of patients in hospitals. Turning over the care of patients in hospitals to these hospitalist physicians would also enable primary care clinicians to spend more time focusing on outpatient care. (Primary care clinicians should certainly see their patients when they are in the hospital, but the time required for managing their care – and traveling to and from the hospital multiple times a day – can certainly limit the time primary care clinicians can spend with their other patients.) This type of “specialization” would increase both the quality and efficiency of care, and could lead to physicians spending more time consulting with patients and ordering less tests and procedures. (See below for trend data in Medicare.) Of course, accomplishing this would require that these hospitalist physicians be given the ability to actively manage the patients in the hospital – something that is not allowed in some hospitals or by some primary care clinicians who insist upon maintaining full management control over “their’ patients.
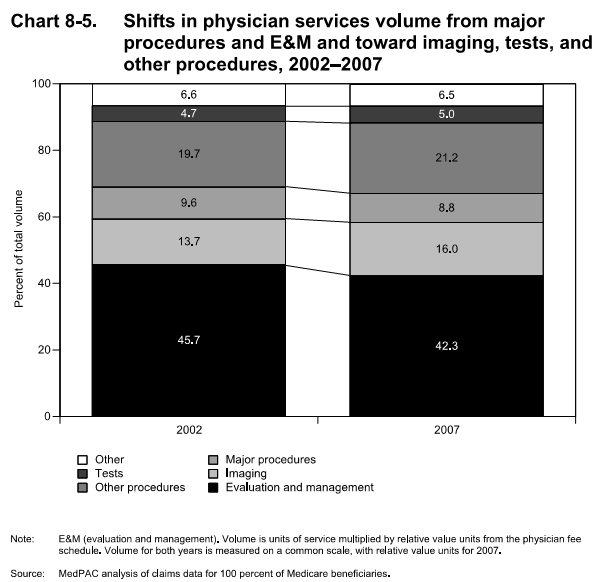
(From: MedPAC June 2009 Data Book.)
Bottom Line & End Result
Shifting the ratio of primary care to specialist clinicians to be closer to 50/50 from the current ~30/70 would provide enough primary care clinicians to deliver primary care services that patients really need. This would also lessen primary care physicians’ time constraints and reduce the pressure for quickly referring patients to specialists. Overall, this would certainly be a better patient-centered healthcare environment for individuals and society. The question is, do we have to wait 20 or so years to get there – which is what it will take through graduating more primary care clinicians from school and training programs – or can steps be taken to shift the system sooner.
These types of reorganizations are not unheard of in other sectors. For example, printing companies have shifted from lead type, to offset, to laser type printing rather quickly, and telephone company employees have gone from dealing with copper wires for voice transmission, to DSL service, to fiber optic cables. These innovations didn’t wait for entire generations to graduate from school. People were retrained, and they were eager to do so because that’s where customers’ demand had shifted. If healthcare delivery can be shifted to a more integrated and coordinated system, then the incentives for providing more and better primary care will follow – and then clinicians, administrators, regulators and payers will have to pay more attention to how what they are providing, selling, regulating, and buying makes sense in a transformed delivery world.

Thanks Christopher – Great comment. I absolutely agree that increasing teamwork – which is critical for successful medical homes – is important, as are initiatives focused on non-physician clinicians such as NPs, PAs, etc. The ACP is advocating for national health care workforce policies, and this should clearly address the entire range of clinicians, like diabetes educators, etc. And the ACP and MedPAC do address non physician supply issues – as does Kaiser Family Foundation. I didn’t get into those policies because most of those clinicians are already working in primary care so expanding their supply is more about increasing training and education slots as opposed to retraining – which would certainly be quicker… Although retention is also an important issue for both physicians and other clinicians, and telemedicine may provide an opportunity for more “experienced” clinicians who may have trouble working in direct clinical settings to continue providing care to locations where services are very limited. I know telemedicine is usually thought of as a tool for specialty services, but it can be used for primary care as well – particularly for remote locations…. which actually reminds me about a discussion I had with someone many years ago about a company that provided medical radio consultations to ships at sea – and of course there was no video component back then.
And lastly, yes, free parking is a very minimal “perk,” but the point is that one of the reasons that medical students are being discouraged from going into primary care is that the current physician/medical culture looks at primary care as the bottom of the prestige pyramid, and medical students get this message either directly or indirectly from their teachers and mentors, so we need to find someway to reverse this. After all, in a reformed delivery system with PCPs coordinating care, they should be viewed as the quarterbacks and/or sideline coaches rather than the blockers and tacklers or equipment managers. (I know the analogy doesn’t hold up completely, but I hope you get the idea, and that nobody in the NFL takes any offense at any of this since they are all a LOT bigger than I am.)
Wow! What an impressive description of the issues facing “delivery system reform” as part of health care reform.
As I’m sure you would agree, some of the proposals for increasing primary care capacity are clearly a bit week – anytime you find yourself using special parking spaces as an incentive you are clearly grasping at straws. But retraining, increasing use of hospitalists, along with better pay, and working conditions (inc. prestige), will at least eventually draw people in.
I did wonder why the proposals don’t include making more use of nurses and others as PCPs. Clearly the need for increased primary care capacity is such that there will be more than enough work for all who want it and there is every reason to believe that NPs and others can deliver quality care in well designed systems.
Which brings me to my last point, “well designed systems.” Not only is primary care weak in the US because it is underpaid, but practices are typically not “designed” to deliver highest quality care, particularly for patients with chronic diseases.
As Ed Wagner’s work over the decades has shown, there are many additional aspects to delivering high quality primary care to a population that is aging and has a high burden of chronic disease. It requires additional skills in patient activation, team work, practice process redesign (even to benefit from the opportunities created by EMRs), and a shift in mindset from reactive episodic care to proactive planned care.
I think we need an even broader agenda for delivery system reform, workforce policy, and training standards, if we are to get the health outcome improvement and cost reductions we are looking for in health reform.