The cost of so-called specialty drugs has become a major health policy issue largely because of spending projections for new medicines for chronic hepatitis C infection and cancers. Having worked on issues related to the development, approval, availability, use, and cost of medical treatments for more than 25 years, I’ve noted with concern and bemusement how cost and value issues are being discussed and presented in public debates and policy circles.
The Intense Debate About New Biopharmaceuticals Was Predictable
The introduction of significant new specialty medicines is reasonably predictable because information about biomedical research and the developmental status of new drugs and biologics is publically available from the FDA and company press releases. And while the specific list prices of new medicines can’t be precisely known before they are approved and launched, with a basic understanding of healthcare economics approximate price ranges are reasonably predictable. (Both of these are discussed below.)
So how does something that was predictable also become so contentiously inflammatory? The intense debates and diatribes about the price and value of new biopharmaceuticals is not surprising because of the rancorous politics surrounding healthcare in the U.S., and the apparent lack of research and foresight by organizations involved with paying for medical care. (Neither of these are discussed below.)
The overall situation seems to boil down to that, as a society, we’ve gotten what we’ve asked for in terms of new treatments based upon billions of public and private dollars invested in biomedical R&D, but we are now very upset with the result. An analogy might be someone who wins a new car on a game show, but is then very surprised and upset because they have to pay income taxes on the value of the car, pay to register the car, pay for insurance, pay for gas, pay for maintenance, etc.
To examine this situation more deeply, let’s step back and look a bit closer at what the new (so-called) specialty medicines are, how we’ve been asking for them, and why they are not generally the fiscal crisis many have been Chicken-Littleing about.
What are Specialty Medicines?
Specialty medicines are not a specifically defined category of medicine or medical therapy. The FDA approves and regulates medicines for human uses in the general categories of pharmaceutical drugs (which are mostly small molecules), biologics (which are mostly proteins or other very large compounds produced in living cells), insulins, vaccines, and blood and tissue products. Across those categories the FDA recognizes orphan medicines as therapies for conditions that affect less than 200,000 people in the U.S. The FDA also has pathways for more rapidly approving new medicines based upon clinical need, as well as for expanding access to experimental compounds prior to FDA approval. There is no category for “specialty drugs.” (And as an aside, there is also no category for “biotech drugs”. Biotechnology is a technology, process or method for conducting research or creating new molecules.)
Similarly, the Centers for Medicare and Medicaid Services (CMS) has extensive provisions for how medicines are covered and paid for under various parts of Medicare (Parts B, D, and C), and Medicaid, but none of those include specific requirements related to “specialty drugs” based upon their molecular structure, method of production, medical use or need, patient population, or any other clinical factor. However, many health insurance plans (including Medicaid programs and Medicare Part D plans), have tiers for expensive therapies labelled “Specialty Drugs.” This bottom line perspective was aptly described in an article[i] in Health Affairs’ October 2014 themed issue on “Specialty Pharmaceutical Spending & Policy”:
“There is no uniform definition of specialty medications. However, there is a consensus that all of them are high cost (Medicare Part D uses a $600 per month threshold for the “specialty” designation), are relatively difficult to administer, require special handling, or require ongoing clinical assessment—or have some combination of these four characteristics. All of the characteristics are routinely used to define specialty medications. However, one recent survey indicated that cost is the dominant factor, with 85 percent of respondents at health plans rating cost as very or extremely important in their decision to assign the specialty designation to a medication.6
The medications that have received that designation are a heterogeneous group. They include small molecules that are produced on an industrial basis, such as dimethyl fumarate (Tecfidera), which is used in the treatment of multiple sclerosis; manufactured human proteins, such as growth hormone; and exquisitely designed monoclonal antibodies (such as trastuzumab) that target cancer cells or help control an inappropriately stimulated immune system (for example, infliximab).”
So the bottom line is the bottom line: Specialty drugs are expensive drugs for which health insurance plans are requiring patients to pay higher co-pay/co-insurance amounts. And those higher financial requirements may be in addition to health plans’ other utilization management requirements such as quantity limits, prior authorization programs, and step therapy (a.k.a. “fail first”) protocols.
Why Specialty Medicines are The Same as Older New Medicines, Only Different (and Potentially Better)
Specialty drugs are expensive medicines – more expensive than medicines approved 10, 20, or 30 years ago, e.g., Prozac®, Epogen®, Invirase®, Lipitor®, Gleevec®, Avastin®. But they are also more likely to be effective, and/or treat conditions that did not have very good therapies. These newer medicines are generally the result of the evolution of biomedical science that is producing more molecularly targeted therapies. This advancement has been supported by public policy to promote more basic and applied research at the National Institutes of Health, academic research organizations, and biopharma companies, which in the U.S. totaled about $120-130 billion in 2012. (Why was has there been longstanding broad political and public support for increasing the NIH’s budget if not to push forward to create new treatments?)
Below is a graphic from the late 1990s that illustrates how biomedical advances have led to newer treatments.
We are now in that period beyond 2005 represented in the upper panel by the large red “?” and the cornucopia of capsules in the bottom panel. That is, we have gotten in the 2000s what we had been asking for and paying for in the 1990s and earlier: Better treatment options.
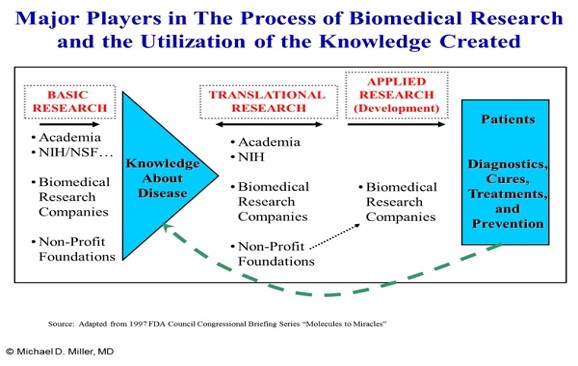
And to expand upon this picture, the graphic below illustrates the major types of organizations involved with biomedical research, and how they interact and influence each other through the exchange of information.
How New Medicines Fit Into Clinical Care
With the newer targeted, molecularly based medicines, there is – by design – a greater match between the pharmacology and the patient’s physiology leading to better outcomes. This means there is a greater likelihood that the treatment will produce a good clinical outcome. More precise matching of pharmacology to physiology also often means that the number of people who should be using the particular medicine is smaller than would have been the case for untargeted medicines developed when there was less understanding of physiology and pharmacology.
Below is a simple diagram (starting in the lower left corner) depicting how clinical decisions are made, and how more effective treatments can improve clinical outcomes.
Overall Value of Innovative Therapies
While any individual medicine may be innovative and provide value, as the “Process of Discovery & Development” figure above illustrates, these advances often involve treating a disease through a new mechanism of action, i.e., moving from one “therapeutic revolution” to the next.
Below is a simplified picture illustrating how the value of medical innovation can increase in several ways:
- By developing a better medicine using an already targeted mechanism of action, e.g., a medicine with reduced or fewer side effects;
- By developing a new medicine that targets a new mechanism of action, a.k.a. a new class of medicine to treat a disease; and
- Research that discovers how an existing medicine can be used to treat another disease, e.g., methotrexate for autoimmune diseases.
Discussed below is how a new medicine’s higher success rate for treating an illness often translates into a greater value and a higher price. Also discussed is why we shouldn’t be surprised that these medicines are expensive, and how our imperfectly regulated market-based healthcare system is responding.
Why Price and Cost of Specialty Medicines are of Concern, but Not Catastrophic
How are prices of medicines determined? In much of the ongoing public debate, basic economic principles are often ignored: Prices in the United States are almost never determined by a product’s or service’s input costs. (The exception for this would be some commodities and highly regulated utilities like water and electricity – but I suspect not cable TV.) Rather, prices – particularly for research intensive products – are determined by fallible humans who model what markets will bear and how intersecting curves and equations parse out an answer for how to maximize short and long-term profits from a new product. This is sometimes referred to as the Net Present Value (NPV), which tries to capture the value of the product taking into account the expected changes in sales and price going forward along with the expected inflation rate and costs associated with production and sales etc. Those calculations include the expected effective life of the product in the market due to replacement by better versions (e.g., computers or cell phones), patent expiration, or, in the case of something unusual like new medicines that can cure chronic hepatitis C infections, the rapid decline in the number of people with the disease.[ii]
Those calculations for biopharmaceuticals are further complicated by the reality that there is no single price for a medicine in the U.S. where legally required discounts to government programs interacts with private sector rebates and reductions. In addition, projected global prices – which may be linked to one another in various ways – must also be considered along with the volume of sales in various countries and regions.
So how is a “price” for “what the market will bear” determined? The calculations leading to a general range for this price (a.k.a. “list price”) includes:
- How the condition is currently being treated or cured, and the price of those treatments (both pharmaceutical and non-pharmaceutical such as surgery), not only for an individual but for successfully treating one person in a population?[iii];
- What other treatments and complications will be avoided, reduced, or encountreed with the new treatment?;
- How many people are expected to use the new treatment?; and
- The seriousness of the condition and how it impacts the lives of people, i.e., is it fatal or not? Does it seriously compromising their quality of life? etc.
All those factors (and others) are included in a description of “what is the value of the new treatment?” That is, the greater the value (particularly compared to other treatment options) the greater the price for a course of treatment because competition between different treatment options does occur – it is just a particularly challenging assessment since it likely includes many personal issues and preferences related to both biology as well as life circumstances. In addition, because of Federal laws that limit price increases after launch, the initial prices for new medicines may be pushed to the higher end of the range described above.
The Good News, Bad News, Good News – and Other Good News Looking Forward
The good news for the health system is that as more targeted medicines with higher success rates are developed for smaller populations, the total cost is probably no more than if the medicine had been priced lower but used by more people – many of whom would have found it ineffective. The corollary good news is that those new medicines are improving and saving lives. (If that wasn’t the ultimate reason for the spending billions and billions on biomedical research, then someone please tell me what it was.) The bad news is that because of the decades of investment in biomedical research, more and more of these new medicines are being developed and approved by the FDA – and the cumulative cost of those new medicines is increasing at a rapid rate compared to overall spending on healthcare and other medicines.[iv]
The other good news is that the increase in spending on healthcare overall has slowed dramatically in recent years, as has spending on medicines in general, which is not surprising since now more than 80% of medicines dispensed are generics. And the ongoing good news is that our imperfect healthcare system is working: As new medicines are approved they compete with their innovative predecessors for market share and on price. (An example of this for chronic hepatitis C started in late 2014 with the introduction of a new multi-pill regimen.)
Similarly, other good news (sort of) is that there is now a regulatory pathway being developed for approving biosimilar medicines that will compete with innovator biologics, which represent a large portion of the so-called specialty drugs. The reason this is only sort of good news is that biosimilar medicines will likely cost 70-80% of the price of the original biologic medicine because biologics are expensive to produce since they are grown in living cells rather than chemically synthesized.
More good news looking forward is that biomedical science is still progressing and the future will likely see better and simpler medicines that will be higher value for patients and society. Some of that value will be in better quality lives for people, and some of that value will be in reduced spending for other healthcare and related services. For example, a medicine that halted progression of Alzheimer’s disease – or any of the other neurodegenerative diseases such as Parkinson’s, ALS, or MS – (or prevented it from occurring, or cured it) would likely be expensive on a per person basis, but it would prevent the need for many other healthcare services, e.g., other medicines with limited effectiveness, services such as physical therapy, medical devices for physical assistance, and nursing and home care. (An historical example of this was how the polio vaccine dramatically reduced expected acute and long-term care costs.)
In addition, while biosimilar medicines are expected to be only 20-30% less expensive than the original biologic medicine, scientists are working on developing small molecule pill-type medicines that are targeted like biologics. (This is already happening for some conditions, such as certain cancers and rheumatoid arthritis, and one report indicated that over 50% of the specialty drugs in the pipeline are high-cost oral medications.[v]) While those targeted pill type medicines are expensive, because they are small molecule medicines, generic forms will eventually be available, which will be 80-90+% less expensive than the original medicine, i.e., significantly less than biosimilar medicines. And of course, oral medicines have less delivery costs compared to injections or infusions – which sometimes require visits to a doctor’s office of clinic. So even if the patient can inject the medicine themselves, a pill also makes taking the medicine easier and eliminates the cost and hassle of disposing of used needles and other materials involved with the injection. (Reducing the hassle – and pain – associated injections may also increase patients’ adherence to the medicine and thus increase its effectiveness.)
However, with the advancement of good news also comes some bad news. For example, with the new hepatitis C treatments, there are some people and programs that are initially in a no-win situation – and this is most clearly seen with people with chronic hepatitis C who are in jails and prisons. These individuals have a right to medical care, the rate of chronic hepatitis C infection in this population is very high (15-20%), and the risk of transmission from one person to another is higher than average (as is the risk of reinfection if someone is successfully cured). All those factors make strong clinical and public health arguments for rapid and universal treatment for all infected individuals in any non-short term corrections populations – as well as treatment for new inmates with chronic hepatitis C. However, corrections organizations have limited and generally fixed budgets making the provision of this care for all the individuals in their facilities over a short time period a fiscal tsunami.
Corrections facilities that are privately run under contract with state and local governments face a particular challenge because, unlike government owned and operated corrections facilities, they are unable to negotiate much lower prices for the new hepatitis C treatments since those discounts wouldn trigger automatic price reductions for state Medicaid (and other ) programs that have legislatively proscribed best price requirements. This means that state and local governments that have contracted out the operations of their corrections’ medical facilities may actually be facing higher costs in the future – at least for medical care for the inmates.
Generating More Good News for the Future
The general relationship between how we pay for medicines today and what treatments and cures we end up with tomorrow is also often missing from debates and analyses of biopharmaceutical costs and treatments. Below is a simple graphic illustrating some of those relationships.
Appreciating these factors is important as we seek to translate basic research into new treatments, and is particularly salient because of the current situation with Ebola treatments – or the lack of them. Specifically, Ebola hasn’t been an illness in a geographic region where there has been extensive access to medical care or doctors, or a way for the people affected to pay for those treatments. (Bottom two items in the top portion of the graphic). Thus, until Ebola became a global and first-world health concern, there has been very low financial incentives for anyone (government or industry) to invest in discovering or developing new/better treatments for Ebola. (Third item in the bottom portion of the graphic).
Conclusions
- Specialty drugs should be called what they are: expensive medicines, treatments or cures. Giving them a group name implies that they have some unique or differentiating characteristic – aside from price or cost – particularly with a word root indicating that these medicines are somehow “special.”
- Healthcare is complicated. Biomedical science is complicated. Healthcare economics is complicated – particularly when many health plans have five (or more) cost-sharing tiers for medicines.
- Biomedical research has produced some incredibly effective new treatments. (Thank you!) However, there are still many serious, chronic, and life-threatening illnesses with few (or zero) good treatment options.
- Prices and value in healthcare are as complicated concepts as biomedical science. And value assessments almost always involve personal factors. For example, would Steve Jobs have paid $1 billion for a cure for his pancreatic cancer? I think so.
- Society has invested billions in biomedical research and development (probably close to a Trillion dollars over the past 20 years), and received significant benefits. The ongoing challenge is how to maximize those and future benefits by making difficult financial, resource, clinical, and ethical decisions within our imperfect healthcare system run by fallible biological beings.
p.s. Sorry for the long post.
[i] “Specialty Medications: Traditional and Novel Tools Can Address Rising Spending on These Costly Drugs,” Lotvin et al., Health Affairs 33, No. 10 (2014) 1736-1744.
[ii] A similar situation happened in the early 1990s with the introduction of new flexible lenses for cataract surgery. There was a tremendous upswing in the number of operations, which cost Medicare much more than expected, due to pent up demand. And after that surge, the number of people getting cataract surgery (and the costs) dropped to a much lower steady state – although one that continued to increase at a small growth rate because of the aging demographics in the U.S.
[iii] For example, if a new treatment successfully treats 50% of people with a serous condition, and the older treatment only successfully treats 10%, the clinical value would be 5-times as great, which would also translate into an economic value that is multiple times the older treatment. Other factors that would affect the value would be the route of administration, side effects, and other services and products required or avoided with the new treatment.
[iv] Studies have estimated that per year spending growth for non-specialty medicines is now less than 4% range, while annual spending for “specialty” medicines is growing in the 10-15% range.
[v] “The Growth of Specialty Pharmacy: Current trends and future opportunities, “ UnitedHealth Center for Health Reform & Modernization, Issue Brief, April 2014, citing: Atheer Kaddis and Stephen Cichy, “Payer Tactics to Manage High-Cost Specialty Drugs in the Pipeline,” AIS Webinar – Specialty Pharmaceuticals, September 2013.


Very interesting discussion. Here’s hoping healthcare continues to develop in a way that can help more people and in more effective ways! Thanks for sharing.